

Benign enlargement of the prostate or benign prostatic hyperplasia (BPH)
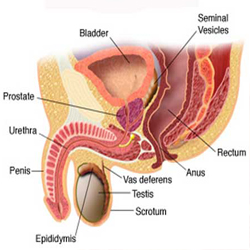
In this condition the prostate enlarges, and as it does so it may compress the urethra (the tube that carries urine from the bladder through the penis) causing problems urinating. It is extremely common, being found to some degree in most men beyond middle age.
BPH can cause various urinary symptoms, known collectively as lower urinary tract symptoms (LUTS) but commonly these include:
 In order to help assess the severity of your symptoms, the International prostate symptoms score (IPSS) can be used. This questionnaire includes a series of questions that ask you about your urinary symptoms and now they affect your quality of life.
In order to help assess the severity of your symptoms, the International prostate symptoms score (IPSS) can be used. This questionnaire includes a series of questions that ask you about your urinary symptoms and now they affect your quality of life.
When you see your urologist, typically you will be asked about your symptoms and medical history, and then he/she will examine you, including a rectal examination to feel the prostate. You should also bring a fresh urine sample with you so that your urologist can do a urinalysis. It is also likely that you will be asked to do a flow rate, which involves you passing urine into a measuring device which then measures the rate at which you pass urine. For this reason you should try and come to the clinic with a comfortably full bladder. Following this, a measurement of residual urine in the bladder will be taken, using a small ultrasound probe placed on the lower part of your abdomen. There are a series of other studies that may be offered. These include:
In order for you to assess how bad your prostate symptoms are, complete the IPSS symptom score sheet and bring it with you to your consultation or take it to your GP. It is also useful to complete a frequency volume chart if you are going to see a urologist. This is a record of the amount of urine you pass each time over a 24 hr period, and usually three days worth of recordings are needed. These days do not have to be consecutive. Please click here for a frequency volume chart.
The symptoms of BPH do not always require treatment. Some men are able to cope with them by altering their fluid intake. Others take medication. If neither of these help, then surgery is usually the best option.
There are two groups of drugs which may be prescribed for patients with BPH. These are alpha blockers, and 5 alpha-reductase inhibitors.
Alpha blockers: These drugs work by relaxing the smooth muscle of the prostate and bladder neck to improve urine flow and reduce bladder outlet obstruction. Although alpha blockers may relieve the symptoms of BPH and improve the flow rate, they do not reduce the size of the prostate. They are usually taken orally, once a day and they work almost immediately. The most commonly prescribed alpha blockers are alfuzosin and tamsulosin. Side effects can include headaches, dizziness, light-headiness, fatigue and ejaculatory dysfunction, but the tablets are well tolerated by the vast majority of men they are prescribed to. These drugs work by relaxing the smooth muscle of the prostate and bladder neck to improve urine flow and reduce bladder outlet obstruction. Although alpha blockers may relieve the symptoms of BPH and improve the flow rate, they do not reduce the size of the prostate. They are usually taken orally, once a day and they work almost immediately. The most commonly prescribed alpha blockers are alfuzosin and tamsulosin. Side effects can include headaches, dizziness, light-headiness, fatigue and ejaculatory dysfunction, but the tablets are well tolerated by the vast majority of men they are prescribed to.
5-alpha-reductase inhibitors (5ARIs): These drugs work by reducing the size of the prostate by preventing the conversion of testosterone to one of its more active metabolites. Two different 5ARIs are available, finasteride and dutasteride. They can relieve BPH symptoms (though they may take upto 6 months to do this) and increase urinary flow rate. Studies suggest that these medications may be best suited for men with relatively large prostate glands. Side effects can include impotence, decreased libido and reduced semen release during ejaculation, but are also rare.
If there is no response to drugs, symptoms can be improved by an operation to core out the prostate gland. At Cambridge Urology Partnership we can perform either a TURP (transurethral resection of the prostate) or a HoLEP (holmium laser enucleation of the prostate), or laser prostate surgery. We also offer minimally invasive treatments such as REZUM and UroLift.
HoLEP stands for holmium laser enucleation of the prostate, and the operation involves coring out the lobes of the prostate which are compressing the urethra. The benefits of HoLEP are the fact that prostate glands of any size can be treated without needing to cut through the skin, the relative lack of complications related to bleeding and fluid absorption compared to conventional TURP (transurethral resection of the prostate), and the decreased length of stay (usually patients only stay one night after their surgery). These benefits have been shown in clinical trials, as has the durability of the operation in removing obstructing prostate tissue when compared to the traditionally recognised “gold standard” TURP.
Tev Aho is one of the most experienced surgeons in the UK in the performance of this type of laser prostate surgery (HoLEP). He trains surgeons from the UK and abroad in the technique, and himself learnt the technique from Mr Peter Gilling, its’ pioneer from New Zealand (see below).
Here’s what the experts have to say about holmium laser prostate surgery for BPH:
“The HoLEP has replaced standard TURP completely and unreservedly in our hospital. There is nothing out there that has been shown to be better.”
Peter Gilling, MD, Consulting Urologist at Tauranga Hospital , Tauranga , New Zealand and holmium laser prostatectomy pioneer:
“Use of the Ho:YAG laser for treatment of BPH is an important new technique that offers significant advantages over TURP….In a phrase, HoLEP compared with TURP provides ‘maximal benefit with minimal morbidity’….I would envision that every significant urology department will have a holmium laser at their disposal. It is a basic tool for stones and BPH, two of the most common conditions urologists treat.“
“HoLEP represents a paradigm shift in the surgical management of BPH and is endorsed by all the leading urological organizations world-wide. We have used this technique exclusively with over 2,000 patients since it evolved in the late 1990’s. Once learned, HoLEP replaces both TURP and open prostatectomy, providing superior outcomes in prostates of all sizes!“
Mr DB, 70yr
“Before the operation I was getting up at least 3 times during the night. I had to urinate very frequently during the day. I knew the location of all the Public Gents in Cambridge and all the pubs where you could use the Gents without buying any beer. Urination flow was poor and incomplete with dribbling. Erections poor and not long lasting. (I was) increasingly very tired and weedy, unable to cycle because of soreness. Everything (was) an effort.
Four months after the operation: Urine flow excellent, with good immediate force, no interruptions and no dribbling. Much longer periods between urination. Some nights I sleep through without wakening. Erections excellent. Much more energy, back to cycling and gardening. I feel as though I have been rescued from poisoning and liberated back to a normal life.
My family join me in thanking you very much indeed for the expert help you gave me during the recent operation.”
Mr BG, 72yr
“My recollection as a young man was being able to pee over a five bar gate onto a mushroom on the other side. However, during the years prior to my operation I found it difficult to pee on to a mushroom six inches from my feet. It gives me great pleasure to now record, following my operation, that I am now able to circumnavigate the above gate once again. Yip-pee!
Within 3 weeks I was playi ng golf again. Within a week I was walking quite briskly and swimming as well. And within 4 weeks I was performing again with my dear wife. I have to record that I was wrong to put off this operation for so long. When I think back at the disturbed nights peeing 3 or 4 times if I was lucky, 3 total blockages when I had to have a catheter inserted, watching out for when and what I had to drink. It really was not worth the delay.
So to Mr Aho and his team very many thanks. You did a splendid job and I shall be eternally grateful.”
Mr HGM, 68yr
Presenting problem: Significant prostate bleeding and very large prostate despite previous prostate vaporisation procedure.
“My experience started some 5000 miles from the shores of the UK. Early one morning I noticed that my urine was bright red. There was obviously something very wrong and I would need urgent medical assistance to stop the bleeding. My local doctors successfully accomplished this but informed me that I would need to have an operation to reduce the size of my prostate.
In the process of deliberation over where this procedure should be done, we discovered through the marvel of the internet the HoLeP procedure (Holmium Laser Enucleation of the Prostate) at the SpireCambridgeLeaHospital, where one of the best HoLEP centres is located. My prostate was about 10 times the normal size. Coincidentally I had earlier been referred to the same hospital to have a cataract operation on both my eyes.
The challenge was whether the consultants and supporting medical staff from two separate disciplines were in a position to coordinate their surgical procedures within a given time scale, particularly as the prostate operation called for prompt action.
All in all, three surgical operations were carried out within an eight day period and I can testify that all were remarkably successful. Throughout the process I experienced little or no pain; and I only spent about three days in hospital. My prostate has been successfully reduced in size and all functions have returned to normal with no side effects. According to my consultant surgeon (Mr Tevita Aho), I should never need to have another intervention for prostate problems.
Finally you may be interested to know that I did not have to mortgage our home or the grandchildren’s inheritance to accomplish this feat. The medical bills were all inclusive, modest in their amount and were easily settled within my credit card limit”
Click here to read the information leaflet about HoLEP
The symptoms of benign enlargement of the prostate do not always require treatment but they can be helped by a number of drugs. If there is no response to drugs, symptoms can be improved by an operation to core out the prostate gland. At Cambridge Urology Partnership we can perform either a TURP (transurethral resection of the prostate) or a HoLEP (holmium laser enucleation of the prostate) HoLEP uses a laser to cut the prostate away from the inside, and it has significant benefits over conventional TURP.
In order for you to assess how bad your prostate symptoms are, complete the IPSS symptom score sheet and bring it with you to your consultation or take it to your GP.
Please click here to download the Frequency Volume Chart