

 Prostatitis is a common condition that may be caused by infection or inflammation of the prostate and sometimes the area around it. It is seen most commonly in men younger than 50 yrs and some studies suggest that as many as 10 percent of adult males suffer from prostatitis. There are several types of prostatitis, each with a range of symptoms. Some men with prostatitis have a great deal of discomfort and pain, which may be in the pelvic area, testicles, or lower back. They may have pain when they urinate or ejaculate. Other patients may have symptoms similar to patients with BPH. Other patients are not really bothered by their symptoms.
Prostatitis is a common condition that may be caused by infection or inflammation of the prostate and sometimes the area around it. It is seen most commonly in men younger than 50 yrs and some studies suggest that as many as 10 percent of adult males suffer from prostatitis. There are several types of prostatitis, each with a range of symptoms. Some men with prostatitis have a great deal of discomfort and pain, which may be in the pelvic area, testicles, or lower back. They may have pain when they urinate or ejaculate. Other patients may have symptoms similar to patients with BPH. Other patients are not really bothered by their symptoms.
Diagnosing prostatitis is challenging, because its symptoms overlap with those of many other conditions. The exact treatment for prostatitis will depend upon which type your doctor thinks you have.
Some men develop chronic prostatitis that keeps coming back again and again. Although not all prostatitis can be completely cured, the symptoms can usually be managed with medical help.
Prostatitis is a common condition that may be caused by infection or inflammation of the prostate and sometimes the area around it. It is seen most commonly in men younger than 50 and some studies suggest that as many as 10 percent of adult males suffer from prostatitis. There are several types of prostatitis, each with a range of symptoms.
Although the causes of prostatitis are not clearly known, there are many theories about why you may contract it. Prostatitis from bacteria may be a result of a backward flow of urine into the prostate. This infected urine may be a result of a recent bladder infection, an abnormality of your urinary tract, a result of a catheterization or recent surgery. Non bacterial prostatitis may be caused by other organisms, or clogging of the prostate ducts. Another theory of the cause of non bacterial prostatitis is that the nerves and muscles around the prostate are not working correctly, and may be causing too much tension at the outflow of the bladder and at the level of the pelvic floor. Also, the nerves in the area of the prostate may have become oversensitive over time, thus causing discomfort and pain in that area. As a result of the causes of non bacterial prostatitis being less well understood, and the symptoms of all the types of prostatitis being very similar, diagnosis and treatment can be a frustrating experience for both the patient and the doctor.
Your urologist will ask you questions about the symptoms you have and are currently experiencing and about your medical history. Please click here to complete a chronic prostatitis symptom score
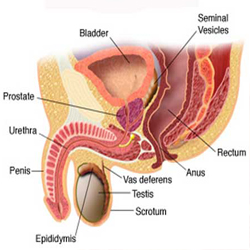
You will then be examined, and this will include an examination of your tummy (abdomen), testicles and a digital rectal examination (DRE) to feel the prostate gland. A urine dipstick will be performed to see if there is any evidence of blood in the urine or of a urinary infection, and the specimen may then be sent off for a urine culture.
Your PSA (prostate specific antigen) blood test may be taken, although the value of this is uncertain.
Your urologist may ask you to perform a flow test to see how fast you pass urine. You will need to have a comfortably full bladder to do this. It involves passing urine as usual, but into a funneled tube which collects the urine and can measure how much you pass per second. Following this you will have a bladder scan, which takes just a minute and involves passing an ultrasound probe over the lower part of your tummy to see how much urine you leave in your bladder.
You may also need to undergo a cystoscopy to examine the prostate and bladder further. This test is completed in the hospital, and takes about ten minutes. A small telescope is inserted into the urethra after an anaesthetic gel is applied. This telescope allows the specialist to see your prostate and bladder, and see if there are any abnormalities or inflammation.
Click here to read our information leaflet about flexible cystoscopy
Treatment of prostatitis depends very much on the cause.
Acute Bacterial Prostatitis
If you are very symptomatic, or sick, you may need to be admitted to the hospital to be treated with intravenous antibiotics. If your symptoms are not severe, antibiotics taken in a pill form can be effective. The antibiotics may be prescribed for upto a month, and it is very important that you take the pills for the length of time prescribed by the doctor. Many men have the tendency to want to stop taking the medication when they feel better, or when their symptoms have gone away. This may result in the infection returning, or becoming a chronic problem. Analgesics or pain medications may be prescribed to relieve pain and discomfort.
Chronic Bacterial Prostatitis
This is also treated by antibiotics, but they are required for one to three months. Again, it is very important that you take the pills for the length of time prescribed by the doctor.
Chronic pelvic pain syndrome
As this form is not caused by bacteria, antibiotics will not help. Your doctor may try antibiotics, initially, however. Treatment of this condition is difficult, and many patients learn how to manage their symptoms. They may find that when they are stressed their symptoms return or worsen, and thus they need to try and learn relaxation techniques. Other triggering factors are mentioned below. The symptoms may wax and wane, or may just appear every few years or so.
A number of other treatments may be tried, and these include:
More natural methods to help symptoms might include:
At Cambridge Urology Partnership, Mr Saeb-Parsy has a specialist interest in this field and works closely with the pain team and specialist physiotherapists to help manage this condition.
Please click here to complete a chronic prostatitis symptom score
Please click here to download our information leaflet
For more information on prostatitis the following sites may be helpful:
The British Prostatitis Support Association
The Prostatitis Foundation (US Based)
Please click here to complete a chronic prostatitis symptom score